The new weight-loss drugs Wegovy and Zepbound are in high demand, and the clamoring will only increase in coming years, experts predict. That’s because drugs like these, which rely at least in part on the appetite-regulating hormone GLP-1, are being investigated not just for weight loss and diabetes, but also for a wide range of other conditions.
“Weight loss is only part of it,” says Dr. Ian Neeland, chair of the American Heart Association’s obesity science committee and an associate professor of medicine at Case Western Reserve University.
Here’s the latest (and still-growing) list.
In March, the U.S. Food and Drug Administration (FDA) allowed doctors to prescribe Wegovy (semaglutide) to reduce the risk of heart attack or stroke in people who are overweight and have a history of heart problems. In one study, people taking Wegovy had a 20% lower risk of heart attack, stroke, or death from a heart event compared to people who didn’t take it.
Some of that benefit to the heart may come from the weight loss itself, since weight can have an adverse effect on the heart. But in the study that Wegovy’s maker, Novo Nordisk, submitted to the FDA, some of the benefits appeared before people began losing weight—suggesting that the drugs are working in other ways to improve the cardiovascular system.
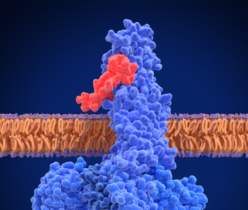
It’s possible that the new weight-loss drugs, which belong to a broader group of hormones called incretins, work directly on fat cells that promote inflammation and contribute to atherosclerosis or narrowing of the blood vessels. “Markers of inflammation drop pretty dramatically in patients taking tirzepatide [Zepbound] in trials,” says Dan Skovronsky, chief scientific officer at Eli Lilly, which makes Zepbound. (Zepbound combines two incretins: GLP-1 and GIP.) “That suggests there may be secondary effects to obesity since visceral fat is inflammatory. That’s exciting to explore.”
Read More: Is Ozempic the New Anti-Inflammatory Wonder Drug?
Lilly is also studying Zepbound’s potential heart benefits by focusing on people with heart failure, since “body mass puts a strain on the heart, and reducing weight should have a profound effect on overall health,” Skovronsky says.
To better understand some of the broader effects that the drugs are having on body, Lilly is also conducting a large trial tracking how Zepbound affects 15,000 people with obesity and their overall rates of a variety of diseases and death. “We are studying death from any cause to see if incretins could have life-saving or life-preserving benefits, which we expect to be true,” Skovronsky says.
Social media is full of stories of “Ozempic babies” that were born to people struggling with infertility who were able to get pregnant after starting GLP-1 drugs for diabetes or weight loss.
Reproductive health experts caution that the connection may not be as direct as people might think. “What would surprise nobody is that getting weight into normal range will promote fertility,” says Dr. Zev Williams, director of the Columbia University Fertility Center. “If that’s through diet, exercise or medications, the net result is that there is a common pathway from reducing obesity to improving fertility.”
Read More: How Researchers Are Working to Make IVF More Effective
Extra weight can lead to abnormal menstrual cycles, which can also make pregnancy more difficult, says Dr. William Dietz, director of the Stop Obesity Alliance at George Washington University. Losing weight could help to restore cycles and increase the chances of pregnancy.
Beyond that, however, incretins could address some of the biological processes involved in fertility. About 10% of women of childbearing age in the U.S. have polycystic ovary syndrome (PCOS), which is the most common cause of infertility. PCOS is a hormone disorder, and it can be driven by insulin resistance or increased levels of insulin in the body. And because insulin is closely tied to weight, controlling weight—and the resulting normalization of insulin responses—could also address PCOS and ultimately a woman’s chance of getting pregnant.
People with diabetes often develop kidney complications. Those taking the drug Ozempic (semaglutide—the same drug as Wegovy—but approved in different doses for diabetes) reduced their risk of dying from either kidney or heart events by 24%, according to data from Ozempic’s maker Novo Nordisk.
Read More: 7 Myths About Kidney Cancer, Debunked
Lars Freurgaard Jorgensen, the company’s CEO, says he anticipates that in coming years, the market for drugs like Ozempic will become more specialized and diverse, due to the wide range of body systems that are affected by weight gain. “Today we look at obesity as one market, but going forward it will be made up of different segments—some people will have obesity and fatty liver, some with obesity and cardiovascular disease, and others with obesity and kidney disease,” he says. “Different products might lend themselves to slightly better outcomes, so we may see more personalized obesity care over time.”
Over time, obesity can lead to the accumulation of fat cells in the liver, contributing to a condition called metabolic dysfunction associated steatohepatitis (MASH). The excess fat causes inflammation that can damage the organ and potentially lead to liver failure. In early studies, Lilly scientists reported that tirzepatide can slow the progression of MASH, possibly preserving liver function. In the study involving 190 people with the condition, 74% receiving the highest dose of the drug (three times the dose for weight loss) were able to clear themselves of the disease after a year, compared to 13% of those receiving placebo.
About 40% of people who have a BMI of 50 or greater also have obstructive sleep apnea, which causes them to stop breathing temporarily. Losing weight can directly lower the risk of sleep apnea, and results from a late-stage study from Lilly showed that tirzepatide led to 30 fewer such events, or a reduction of 63%, each hour for people with obesity and the sleeping disorder. The drug could be “practice changing” for these patients, says Skovronsky, since there are no effective medications currently available, and most people rely on CPAP machines and other cumbersome and inconvenient devices.
Read More: Why Waking Up Earlier Isn’t Necessarily Better
Excess weight has a damaging effect on joints and can alter the body’s fat-to-muscle ratio, so losing weight may also impact the muscles and skeletal system. Researchers are studying whether incretins, which can reduce inflammation, represent a new group of potential treatments for conditions like osteoarthritis, in which joints deteriorate as inflammation flares up.
Weight gain can also lead to changes in the brain, including increasing inflammation that can affect nerves. But research also suggests that incretins can have direct effects on brain pathways, in particular those involved in the reward system implicated in addictive behaviors. Studies in animals show that incretins, and GLP-1s in particular, can dampen brain signals associated with reward and addiction, and lead to lower intake of alcohol and addictive drugs. Scientists are now studying whether the same effects occur in people.
The range of conditions impacted by incretins hints at the potential power they may have in addressing a number of chronic diseases—and that’s not lost on the scientists developing the next generation of these drugs, which combine multiple incretins. The goal also includes shifting these from injections to pills to make it more convenient and accessible to more people.
The many conditions implicated by the medications are “a good reminder of how important metabolism is for overall health, and it impacts our risk for disease,” says Skovronsky. “It’s something we knew but were never able to improve with pharmacology. Now we can, so seeing all the benefits that could occur is super exciting.”
Contact us at letters@time.com