Advertisement
Supported by
Public employees in West Virginia who took the drugs lost weight and were healthier, and some are despondent that the state is canceling a program to help pay for them.
Reporting from Pineville, Charleston and Morgantown W.Va.
Joanna Bailey, a family physician and obesity specialist, doesn’t want to tell her patients that they can’t take Wegovy, but she has gotten used to it.
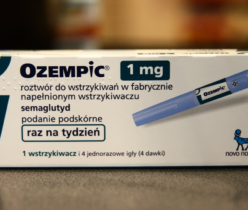
Around a quarter of the people she sees in her small clinic in Wyoming County would benefit from the weight-loss medications, which also include Ozempic, Zepbound and Mounjaro, she says. The drugs have helped some of them lose 15 to 20 percent of their weight. But most people in the area she serves don’t have insurance that covers the cost, and virtually no one can afford sticker prices of $1,000 to $1,400 a month.
“Even my richest patients can’t afford it,” Dr. Bailey said. She then mentioned something that many doctors in West Virginia — among the poorest states in the country, with the highest prevalence of obesity, at 41 percent — say: “We’ve separated between the haves and the have-nots.”
Such disparities sharpened in March when West Virginia’s Public Employees Insurance Agency, which pays most of the cost of prescription drugs for more than 75,000 teachers, municipal workers and other public employees and their families, canceled a pilot program to cover weight-loss drugs.
Some private insurers help pay for medications to treat obesity, but most Medicaid programs do so only to manage diabetes, and Medicare covers Wegovy and Zepbound only when they are prescribed for heart problems.
Over the past year, states have been trying, amid rising demand, to determine how far to extend coverage for public employees. Connecticut is on track to spend more than $35 million this year through a limited weight-loss coverage initiative. In January, North Carolina announced that it would stop paying for weight-loss medications after forking out $100 million for them in 2023 — 10 percent of its spending on prescription drugs.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in.
Want all of The Times? Subscribe.
Advertisement